Introduction:
The field of medical informatics can be traced back to the late 1960s when automated instruments (SMA12 Technicon Sequential Multiple Analyzer 12 Channel) and laboratory systems started to populate hospital clinical labs. These were based on small minicomputers that used machine language and basic programming. These early systems performed small tasks like peak finding and report generation. Fast forward over fifty years to our modern day EMRs (electronic medical records) running thousands of hospitals and clinics across the country. This digital transformation has been fueled by billions-of-dollars of government funding and produced a few giant billion-dollar corporations that now control the medical informatics market. What have all these funds and all this technology accomplished and are we better now than we were back then?
Discussion:
A watershed article was recently published that takes a serious critical review of the American EMR experiment. This article appears in the 2019, April edition of Fortune magazine. The title is; “Botched Operation”. The authors Erika Fry and Fred Schulte took a serious look at this massive change in our healthcare delivery system and have some very powerful comments to deliver. I encourage anyone who has an interest in this field to read the whole article because it has truth that others do not want you to hear.
My job in this short editorial is to highlight the conclusions of their study and try to offer ideas about a next step to fix the problems they uncovered.
1. Government approved EMRs are being sold and used that were never adequately tested or validated before use. Law suits have proven system errors and malfunctions that cause serious human suffering and death. Our tax dollars (in-the-billions) paid for these systems. Over 90% of American hospitals and clinics now use these government “approved” systems. The VA is the next huge system to step into this EMR mix and they will have no better results that what already has happened.
2. Our $3.7 trillion-dollar healthcare system is now totally controlled by these EMRs. The government has recently invested $36 billion dollars into EMRs and there is now great concern over the value of this tremendous leap of faith. We have a healthcare system that is now enslaved to these EMR vendors with little control over their behavior or what physician’s need and want. The hospitals are locked into these systems since their entire accounting system is run through their EMR software. This makes it very difficult to change vendors.
3. These new systems have not reduced costs but have automated upcoding to increase hospital and clinic revenue. These additional costs are covered by the government and insurance carriers. That means that the consumer pays more in taxes and premiums.
4. These EMRs are consuming an inordinate amount of physician and staff time in documenting and clicking their way to an automated bill. These EMRs are optimized for billing and not for patient care.
5. These EMR companies and the government have secrecy clauses in their contracts that limit the ability of hospitals and doctors to point our errors and problems with these systems. A “shield of silence” is protecting these systems.
6. These EMRs don’t share data and the health records of patients are not available to the average patient. You get lab data and that is usually it. These systems are all designed differently and can’t communicate with each other. This was the result of a rush by the government to spend the money before prototype testing and validation.
7. The average outpatient encounter time is now about 10 minutes and a majority of that time is spent on the EMR clicking thru the hoops of government mandated screens. The goal is to bill for the highest amount possible “under the law”. The average ER doctor will need to do 4000 mouse clicks during his shift to complete his medical records. Even then he may not be finished with his EMR clerical duties.
8. These new EMRs are not smart but lack detailed medical knowledge and diagnostic tools. They allow free text to be used or pasted (80%) into the charts to expedite charting. There are no internal prompts to oversee the diagnosis, proper use of tests, and medications. There is no standardization of terminology or symptom reporting. In contrast, the pharmacy portion of these EMRs is totally under the control of a massive pharmaceutical database that stores dosages, delivery, and formulations. The medical part of these EMRs is without this critical database of essential medical knowledge and it will never be consistent or connective without it because there is no standardization.
9. The safety claims against these new EMRs is growing exponentially. There were almost 4000 patient safety cases reported in 2018 and this was said to be very underreported. The government doesn’t even mandate reporting of these EMR patient safety cases.
10. The human interface to these EMRs is also a serious problem. There is now too much data and the screens are not optimized for critical thinking. Errors can be made by long lists and clicking the wrong box. There is no auditing that is being done by the software to detect these mistakes and correct them. These systems also do not allow outside input from a cell phone or external digital device. The whole realm of graphics is now limited to a closed EMR that makes the physician seem powerless.
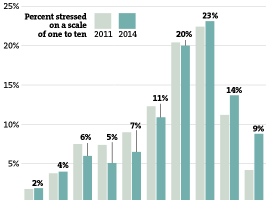
11. Physician and medical staff burnout is at an all time high. Recent studies have been published on this area and it points to the total dissatisfaction of the healthcare staff with these digital cages (EMRs) they must work within (AJM, Vol 131, August , 2018). You can’t practice medicine today and interface with the payors without an EMR. 40-50% of all physician time is spent on the EMR and getting a billable record done. You don’t get paid without it.
What are we now?
1. These billion-dollar EMR companies will not currently rework their physician and staff interfaces because of the costs and retraining required.
2. We don’t have any good intelligent EMRs to prototype against the current systems. The government is not funding this work or encouraging research in this area.
3. There are no recognized national medical databases that can feed these EMRs and make them intelligent.
4. We are currently stuck with commercial control of the healthcare system and in turn the entire medical community.
Any Options?
1. In a competitive market, the products improve because of innovation and technical upgrades. With the huge risks involved in switching to a better product, these EMR vendors are protected and have little incentive to upgrade their product or make a better human interface. We need to introduce competition back into the EMR market and begin testing some intelligent EMRs in the outpatient area where the costs and changes are minimal.
2. We need to encourage the integration of relational medical databases into these intelligent EMRs so that standardization of terminology and symptom format can be done.
3. These intelligent EMRs need to incorporate medical decision support tools so that the process is prospective and integrated into the charting exercise. Let’s fix the problem before it happens.
4. We need to seriously study the human interface that surrounds the patient encounter. We need a new design of office facilities that allows for patient participation in the exam/hospital learning experience. Stop wasting the patient’s time in the office exam room and use this time to teach them how to be good patients and treat their disease.
5. We need to explore new ways to empower the patient to be proactive about their diagnosis and treatment options. The building of intelligent medical avatars is now a real possibility and the tools exist to do this. Every consumer on the planet should have this app on their cell phone and be able to use if for their personal needs. We all know that we don’t have enough medical staff to deal with the explosion of demand that is coming with the rapid increase in chronic disease and diabesity (diabetes and obesity). This means people will need to be proactive for their own and their family’s healthcare and not depend upon an overburdened system to handle all their healthcare requirements.
Conclusion
The United States has made a huge investment in EMRs and it would be wonderful if these wealthy companies would be willing to do the basic research for the next generation system. So far, that has not happened. If necessary, this should be encouraged by government funding to begin this process. HHS has recently called for comments on their EMR policy changes by asking for comments on: 21st Centuries Cures Act: Interoperability, Information Blocking, and the ONC Health IT Certification Program. There are no guarantees that this will actually produce a workable solution and it still depends on the vendors to get this thing right. As a physician, observer, participant, and developer in this industry for over 50 years, I say we can be much better than we are, and all the tools exist to make this possible. Will anybody in power get a vision for a better product and more user satisfaction? We all await your arrival.
|
 Too many doctors have lost hope. Their view of the practice of medicine has changed drastically in the last ten years. They started with a passion to make a difference in the world, to make positive impacts on the health and well-being of their patients. They hoped that their practice of medicine would be preventive, instead of reactive. Heck, some even dreamt of saving lives! The relationship between a doctor and a patient is supposed to be personal, intimate, and, dare I say, enjoyable. But that’s rarely what doctors and patients experience nowadays.
Too many doctors have lost hope. Their view of the practice of medicine has changed drastically in the last ten years. They started with a passion to make a difference in the world, to make positive impacts on the health and well-being of their patients. They hoped that their practice of medicine would be preventive, instead of reactive. Heck, some even dreamt of saving lives! The relationship between a doctor and a patient is supposed to be personal, intimate, and, dare I say, enjoyable. But that’s rarely what doctors and patients experience nowadays.
Some of the biggest complaints I hear from patients today are that:
• They wait for hours to see the doctor, but the visit itself lasts less than five minutes.
• The doctor seems preoccupied with a new electronic medical record system and is often glued to a computer screen.
• The computer injects limitations and roadblocks to needed drugs and procedures, which must be approved by an invisible third party.
• The doctor seems overbooked and overworked, with no time for a really personal relationship.
• There always seems to be an issue with insurance or with uncovered costs.
Full Article...
|
 Please tell me what’s wrong!
Please tell me what’s wrong!
“The Internet keeps telling me I’m going to die.”
Maybe you don’t even know what your medical problem is or don’t have the money to find out?
“Every single time I don’t feel well or my skin develops some sort of weird rash, the first place I go to learn more is Google. I type in my most severe symptoms, and a handful of medical websites, like WebMD, pop up with a few results each. Typically, I don’t worry too much about what these websites suggest, because I’m a young, healthy, 29-year-old male. But when I read what some ‘symptom checkers’ say my likely diagnosis is, my heart jumps a beat. Their suggested diagnoses always sound so severe! They’ll say I probably have some highly contagious and potentially life-threatening disease and that I’ll need to see a medical doctor right away. Of course, when I do see a doctor, my problem is never that severe. Sheesh! Stop scaring me, Internet.”
Full Article...
|
 In a galaxy far, far away, Yoda is in a rush leaving his home so that he can impart more of his wisdom onto Luke Skywalker.
In a galaxy far, far away, Yoda is in a rush leaving his home so that he can impart more of his wisdom onto Luke Skywalker.
Yoda holds down the home button of his android phone and says, “Call Luke Skywalker You Will”
His mobile phone responds with, “Calling Darth Vader”
Yoda freaks out, drops everything in his hands, and takes out his light saber to destroy the phone.
“Whew, close one that was.”
This scenario has happened one too many times. So why do our mobile phones do this to us?
Full Article...
|
 After two decades in practice, the Fergus Falls doctor was a pillar in his community. He was well-off, he was known at the grocery store and the gas station, and he was treating the children of people who had themselves been his patients years earlier.
After two decades in practice, the Fergus Falls doctor was a pillar in his community. He was well-off, he was known at the grocery store and the gas station, and he was treating the children of people who had themselves been his patients years earlier.
And it was killing him.
The pediatrician worried that he was out of touch with the latest methods, that perfection in his practice was impossible, and that he would soon get another late-night call — maybe this time about a child who drowned, or died of smoke inhalation.
“I literally saw every way a kid could get killed,” he said.
Full Article...
|
 When faced with a strange ache or rash, many of us turn to the Internet for a diagnosis, rather than a doctor. That rarely goes well. (It’s Rocky Mountain spotted fever! No, shingles! Leprosy?) To ensure that at least some credible information rises to the top of the results page, Google recently added a medical component to Knowledge Graph, its new research tool. Search for one of the 400 or so medical topics included in the Graph, and a set of facts vetted by a team of doctors and experts will appear in a big box on the right side of the screen.
Full Article...
When faced with a strange ache or rash, many of us turn to the Internet for a diagnosis, rather than a doctor. That rarely goes well. (It’s Rocky Mountain spotted fever! No, shingles! Leprosy?) To ensure that at least some credible information rises to the top of the results page, Google recently added a medical component to Knowledge Graph, its new research tool. Search for one of the 400 or so medical topics included in the Graph, and a set of facts vetted by a team of doctors and experts will appear in a big box on the right side of the screen.
Full Article...
|
New surgery in Israel --How exciting. This is quite remarkable. The
future of medicine from Israel.
I hope this becomes available in all countries and medical centers in
my lifetime! What an innovation.
If you haven't seen this before it is well worth your time to see what
is happening in new methods of surgery
Full Article...
|
Gordon Robertson takes a look at some of the medical breakthroughs that have come from Israel, including cancer and diabetes treatment and technology to help blind people see and crippled people walk.
Full Article...
|
When Dr. David Newman-Toker was a medical resident at a Boston hospital, he witnessed what he calls tragic cases in which otherwise healthy people suffered serious consequences from misdiagnoses that could have been prevented.
Newman-Toker, now an associate professor of neurology at the Johns Hopkins University School of Medicine, recalls an 18-year-old aspiring Olympic skater who fell on a ski slope and came to the hospital with weakness on one side of her body and a headache. She was told she had a migraine and was sent home. Six days later, she returned to the hospital after a stroke compromised the entire right side of her brain. He also remembers a hardworking janitorial immigrant in her 50s who came in with chest pain. She was seen multiple times at multiple hospitals and everyone missed that her chest pain was caused by compression from her spinal cord. By the time it was recognized, she was a paraplegic.
Full Article...
|
It happened on flight from Washington, DC to San Diego.
The pilot’s urgent question reverberated over the intercom during a cross country flight, “Is there a doctor on board?” A passenger was experiencing severe chest pains, and luckily for him Dr. Eric Topol was sitting in seat 6A.
Topol is the energetic chief academic officer of Scripps Health, a prominent cardiologist and the foremost figure in the field of wireless medicine. He believes the future of health lies in our own hands, namely in our smart phones and other portable electronic devices. According to Topol, “the smart phone will be the hub of the future of medicine. And it will be your health-medical dashboard.”
That day on the airplane, Dr. Topol displayed the potential of wireless medicine when he snapped an AliveCor device onto his iPhone and performed a cardiogram at 30,000 feet. Using this portable, cellphone powered device, Topol was able to see that the passenger was definitely having a heart attack and he recommended an urgent landing. The passenger was rushed to the hospital and survived.
Full Article...
|
According to a recent research report from Deloitte, over the next 10 years, mobile health (mHealth) devices will save the healthcare industry $305 billion in increased productivity due to "reduced travel time, better logistics, faster decision-making, and improved communications." Remote home monitoring, authors of the report say, will save the industry nearly $205 billion in the same time period.
The report, mHealth in an mWorld: How mobile technology is transforming health care, looks at what is driving mHealth adoption and where there are additional opportunities. All in all, the researchers say that after a slow start, mHealth is becoming increasingly adopted and accepted as a way to manage and target chronic conditions, capture patient data, and share patient records, among other things.
Full Article...
|
Smartphones and tablets have fundamentally changed how we communicate, get information and conduct commerce. That popularity of apps has carried over into the health care industry as consumers search for easy-to-use mobile apps for health information and caregiver connectivity, and providers scramble to deliver consumer-friendly mobile services to sign on new patients and solidify relationships with existing ones. Case in point: Juniper Research predicts that consumers worldwide will download 44 million health apps in 2012, with continued growth resulting in 142 million downloads in 2016.
Full Article...
|
If some pundits are right, 80% of doctors will find themselves replaced by machines in the 21st century. What kind of machines? Well more a combination of hardware and a big dollop of software to create iDoctors, computers backed by Internet-based datasets with artificial intelligence front ends and powerful analytical capability. Like Watson, the machine that whipped two human trivia champions on Jeopardy, these iDoctors would feature computers as far removed from the laptop, tablet or desktop system you are using to read this blog. They will be minimally multiple-arrayed parallel processors, and later on neuromorphic computer systems. They will be able to assess a patient through observation and questioning. They will then suggest suitable tests, evaluate the results, make a diagnosis and come up with recommended treatment. They will be able to do this with minimal medical supervision and only if surgery or complex treatment is prescribed will require human second opinions.
Full Article...
|
Poorly trained doctors are making wrong diagnoses and dishing out outdated or even incorrect treatment in large parts of India, according to a study
The article in Health Affairs journal detailing the results of a scientific study performed recently in India (The Hindu,December 6, 2012 ) serves to underline what has long been suspected but rarely articulated or discussed on meaningful fora — Just how much do our doctors know? How accurate are they in making a diagnosis and how appropriate is the treatment they recommend?
If the study is any indication, the answer should be alarming. In Delhi, the rate of correct diagnosis was as low as 22 per cent and the rate of correct treatment was less than 50 per cent. This meant that patients in this study had only a one-fifth chance of having their disease diagnosed correctly and less than half got the correct treatment. The study focussed on primary care providers and in rural Madhya Pradesh it has found that in 42 per cent of the cases, unnecessary or even harmful treatment was prescribed.
Full Article...
|
There is a downside to too much information and that is confusion and information paralysis. Google any health term and you’re likely to find millions of search results but for the average person where do they start and whom do they believe ? The internet was supposed to make healthcare choices easier by empowering patients but in some cases it actually could be do more harm than good.
The practice of medicine. We keep hearing that term but what does it really mean ? It means that physicians have to ask a lot of questions and evaluate the “whole” patient in order to form the correct diagnosis. The idea that a doctor can enter some symptoms into a database and have a computer spit out a diagnosis and treatment is pure BS. The more patients physicians see, the better they become at practicing medicine and while empowered patients can help manage their health via the web it should not and cannot be a replacement for a physician-patient relationship.
Full Article...
|
Physicians, including pathologists, will be able to see a more holistic picture of the mechanisms of disease using sophisticated computer-generated models
Medical diagnosis and treatment will be greatly influenced by the fast-growing field of computational medicine. It is a development with the potential to significantly change how physicians use clinical laboratory tests and anatomic pathology services.
Computational medicine describes how researchers are using sophisticated software tools to map highly complex biophysical and disease pathways. This cutting-edge imaging technology enhances their ability to decipher the complex, often non-intuitive dynamics of human disease.
Full Article...
|
Mobile Health (“mHealth”), the use of mobile technology to deliver healthcare services and information, skyrocketed in 2012. 44 million health apps will have been downloaded by the end of the year (predicted to reach 142 million downloads by 2016), and consumers are now spending $700 million per year on these apps. There are over 10,000 health apps in the iTunes app store, the number of American using smartphones for health information grew from 61 million to 75 million this year, and 88% of doctors would like patients to monitor their health at home.
So what are some of the top medical and health apps we’ll be using in 2013?
Full Article...
|
 I recently interviewed author and inventor Ray Kurzweil about his new book, “How to Create A Mind: The Secret of Human Thought Revealed.” The 58-minute segment aired on December 1, 2 and 3 on the C-SPAN2 program “After Words.” The book’s thesis is that it is essentially possible to reverse-engineer the human brain to create a computer mind that works like yours and mine. The advantages of such a creation, Kurzweil told me, are three-fold. First, we can gain an improved understanding of the brain so that we are better able to fix problems with it—for example, developing new treatments for psychiatric and neurological disorders. Second, biologically inspired, more intelligent machines can help us solve numerous practical problems. Third, such a brain-replica may help us understand ourselves, and ultimately to help us become more intelligent. “We are a human machine civilization and we create these tools to make ourselves smarter,” he says. (Hear this response at about 13 minutes.)
Full Article...
I recently interviewed author and inventor Ray Kurzweil about his new book, “How to Create A Mind: The Secret of Human Thought Revealed.” The 58-minute segment aired on December 1, 2 and 3 on the C-SPAN2 program “After Words.” The book’s thesis is that it is essentially possible to reverse-engineer the human brain to create a computer mind that works like yours and mine. The advantages of such a creation, Kurzweil told me, are three-fold. First, we can gain an improved understanding of the brain so that we are better able to fix problems with it—for example, developing new treatments for psychiatric and neurological disorders. Second, biologically inspired, more intelligent machines can help us solve numerous practical problems. Third, such a brain-replica may help us understand ourselves, and ultimately to help us become more intelligent. “We are a human machine civilization and we create these tools to make ourselves smarter,” he says. (Hear this response at about 13 minutes.)
Full Article...
|
The United States will require at least 52,000 more family doctors in the year 2025 to keep up with the growing and increasingly older U.S. population, a new study found.
The predictions also reflect the passage of the Affordable Care Act -- a change that will expand health insurance coverage to an additional 38 million Americans.
"The health care consumer that values the relationship with a personal physician, particularly in areas already struggling with access to primary care physicians should be aware of potential access challenges that they may face in the future if the production of primary care physicians does not increase," said Dr. Andrew Bazemore, director of the Robert Graham Center for Policy Studies in Primary Care and co-author of the study published Monday in the Annals of Family Medicine.
Full Article...
|
 Machines will replace 80 percent of doctors in a healthcare future that will be driven by entrepreneurs, not medical professionals, according to Sun Microsystems co-founder Vinod Khosla.
Machines will replace 80 percent of doctors in a healthcare future that will be driven by entrepreneurs, not medical professionals, according to Sun Microsystems co-founder Vinod Khosla.
Khosla, who wrote an article entitled Do We Need Doctors Or Algorithms? earlier this year, made the controversial remarks at the Health Innovation Summit in San Francisco, hosted by seed accelerator Rock Health. The article had already touched on some of the points of his keynote speech, however it was at the summit that the investor challenged a room full of doctors to disagree with his argument -- a challenge that was met with silence. Either the collection of professionals -- that included fellow speakers Andy Grove, Intel's former CEO, and Thomas Goetz, executive editor of Wired US -- were too horrified by a future where patient care is sacrificed for efficiency, or maybe, just maybe, they realised Khosla was speaking a lot of sense and that the healthcare system in its current state will, one day soon, be rendered redundant.
Full Article...
|
Information technology is now indispensable to the success of your organization. Market leaders are those who best take data and turn it into actionable and strategic information. How well data is harvested and information managed will define winners and losers.
As Jim Collins succinctly puts it, “IT is never the reason for an organization’s success or failure, but can be the accelerator of either.” Prosperous and transformative healthcare requires IT-enabled business solutions. Clinical science and modern reforms are increasingly complex.
The grace period is over. We need CEOs and CIOs who understand this concept and who then jointly execute to make this a reality.
Full Article...
|
Sherlock Holmes would be proud of IBM's Watson computer. No longer the bumbling sidekick portrayed by Arthur Conan Doyle, the supercomputer has managed to master natural language skills, defeat Jeopardy contestants, and wow medical school professors with its potential to diagnose esoteric diseases. I suspect it would even make the late IBM President Thomas J. Watson, for whom the computer is named, proud.
Working with medical researchers at Columbia University, IBM is inputting data from medical textbooks and journals to create a diagnostic engine unlike any in the world. But it's likely we won't see a commercially available product for perhaps two more years.
Full Article...
|
|